Understanding Disc Prolapse
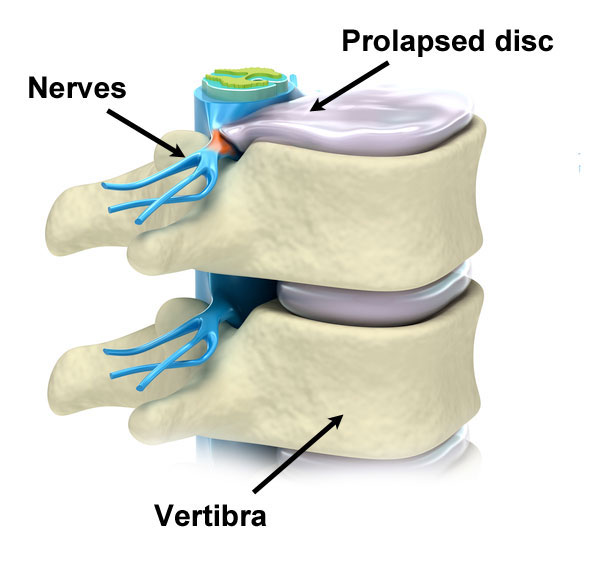
Disc prolapse, commonly known as a herniated disc, is a medical condition where the soft inner portion of a spinal disc pushes through a tear in its tougher exterior casing. This can result in pain, weakness, and numbness, often affecting the lower back or neck. Understanding the intricacies of this condition is pivotal for timely diagnosis and treatment.The intervertebral discs act as cushions between vertebrae, providing flexibility and shock absorption. However, factors such as degeneration, trauma, or improper lifting can compromise their integrity, resulting in herniation. Recognizing the underlying mechanisms and symptoms of disc prolapse is essential for timely diagnosis and intervention, ensuring effective management and relief.
Causes of Disc Prolapse
Disc prolapse, or herniated disc, arises primarily due to degenerative changes in the spinal discs over time. As individuals age, the discs lose their elasticity and fluid content, making them susceptible to tears and herniation. Traumatic injuries, such as sudden impacts or falls, can also precipitate disc prolapse by exerting excessive pressure on the spinal discs. Additionally, repetitive strain from activities involving heavy lifting, twisting motions, or poor posture exacerbates wear and tear on the discs, heightening the risk of herniation. Furthermore, genetic predisposition and underlying structural abnormalities in the spine can contribute to disc prolapse, underscoring the multifactorial nature of this condition.
Recognizing Symptoms
In the realm of disc prolapse, recognizing symptoms is pivotal for timely intervention. Localized pain serves as a primary indicator, often manifesting in specific areas of the back, neck, or extremities, with pain commonly radiating down the leg or arm. Concurrently, muscle weakness becomes evident, particularly in regions innervated by the affected nerve, leading to diminished strength and functionality. Additionally, individuals may experience tingling or numbness, characterized by a pins-and-needles sensation, indicative of nerve compression or irritation. This neurological manifestation underscores the urgency of addressing the underlying issue. Furthermore, limited mobility emerges as a significant concern, as individuals grapple with restricted movement, particularly in bending, twisting, or performing routine activities. Recognizing these multifaceted symptoms empowers individuals to seek medical evaluation, facilitating targeted interventions and fostering enhanced quality of life.
Diagnostic Procedures
Accurate diagnosis plays a pivotal role in understanding the severity and location of disc prolapse, guiding subsequent treatment strategies. Among the foremost diagnostic procedures employed is the Magnetic Resonance Imaging (MRI) scan, a non-invasive technique offering detailed images of soft tissues, including spinal discs. This imaging modality provides unparalleled clarity, enabling healthcare professionals to discern the extent of herniation and its impact on adjacent nerves. Additionally, Computed Tomography (CT) scans may be utilized to capture cross-sectional images of the affected area, offering insights into bone structures and potential nerve impingements. Furthermore, X-rays can provide a broader view of the spinal column, highlighting any abnormalities or degenerative changes. Collectively, these diagnostic procedures empower clinicians to formulate a targeted treatment plan, ensuring optimal outcomes and patient well-being.
Treatment Modalities
Conservative Approaches
various treatment modalities aim to alleviate symptoms and restore functionality. Physical therapy stands as a cornerstone in the conservative management approach. Through targeted exercises and rehabilitative techniques, physical therapists enhance spinal strength, flexibility, and posture. This not only alleviates pain but also fosters long-term spinal health, enabling patients to regain mobility and functionality.
Pain management plays a pivotal role in mitigating the discomfort associated with disc prolapse. Medical practitioners may prescribe nonsteroidal anti-inflammatory drugs (NSAIDs), muscle relaxants, or corticosteroid injections to alleviate acute pain and inflammation. Additionally, alternative therapies like acupuncture or transcutaneous electrical nerve stimulation (TENS) offer non-pharmacological pain relief modalities.
Furthermore, emphasizing rest and relaxation remains integral in the treatment paradigm. Limiting strenuous activities and adopting periods of rest facilitate tissue healing and alleviate undue stress on the affected disc. Incorporating ergonomic adjustments and adopting proper posture further augments the efficacy of restorative measures, promoting optimal recovery and minimizing recurrence risk.
Surgical Interventions
In cases where conservative treatments prove ineffective, surgical intervention may be warranted. Discectomy, laminectomy, and spinal fusion are among the surgical procedures aimed at alleviating pressure on the affected nerve and restoring functionality.
Prevention Strategies
Maintain Proper Posture
Maintaining proper posture is paramount in averting disc prolapse. When sitting or standing, aligning the ears, shoulders, and hips in a straight line reduces undue stress on spinal discs. Utilizing ergonomic chairs and adjusting workstation height ensures optimal spinal alignment, mitigating the risk of injury.
Exercise Regularly
Regular exercise is pivotal for fortifying spinal health. Engaging in activities such as swimming, walking, or yoga enhances flexibility and strengthens core muscles, providing vital support to the spine. Incorporating a balanced exercise regimen not only alleviates strain but also promotes overall musculoskeletal wellness.
Lift Safely
Adopting safe lifting techniques is essential to prevent disc prolapse. Prioritize bending the knees, maintaining a straight back, and lifting objects close to the body. Distributing weight evenly and avoiding sudden, jerky movements minimize strain on the spine, safeguarding against potential injuries.
Ergonomic Considerations
Embracing ergonomic considerations in daily activities significantly diminishes prolapse risk. Investing in supportive furniture, such as chairs with lumbar support, and arranging workspaces to facilitate natural movements fosters spinal health. Moreover, utilizing adjustable desks and ergonomic accessories promotes comfort, reducing the likelihood of strain-induced disc complications.
Incorporating these prevention strategies proactively fortifies spinal resilience, ensuring optimal health and functionality.
Conclusion
Disc prolapse, though a prevalent condition, necessitates comprehensive understanding and proactive measures for effective management a
In conclusion, understanding disc prolapse is crucial for timely intervention and prevention. Recognizing its causes, such as degenerative disc disease and poor posture, allows for proactive measures like physical therapy and ergonomic adjustments. Effective treatment modalities range from conservative approaches like pain management to surgical interventions when necessary. Emphasizing proper posture, regular exercise, and safe lifting practices can significantly mitigate the risk. By adopting these strategies and maintaining spinal health, individuals can enhance their overall well-being and quality of life.
Ready to explore your options for chiropractic and physiotherapy? Contact SwastyaPhysio today to schedule a consultation and discover the best path to your wellness journey. We’re here to support your health every step of the way.
Banaswadi | HBR layout | Kalyan Nagar | Kammanahalli | Horamavu | Hennur